Why choose an EMS DolorClast® shockwave therapy device?
- Jonathan Hall

- Jan 10
- 10 min read
Not all shockwaves are equal and the science matters.
If you’re looking for an osteopath or specifically an osteopath on the North Shore offering shockwave therapy for conditions like plantar fasciitis treatment Auckland or Achilles tendinopathy treatment Auckland, it’s important to know this:
Shockwave therapy is only as effective as the device delivering it.
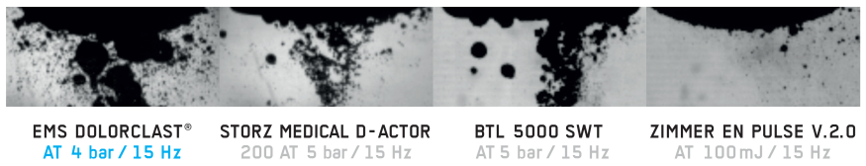
While many clinics advertise “shockwave”, the biological effects depend on the physics of the wave itself. Different machines deliver very different pressure profiles, energy stability and tissue effects – even when the settings on the screen look similar.
At Movement Mechanics, we use EMS DolorClast® shockwave systems because they are among the most extensively studied and acoustically characterised devices available. This matters for both patients and referring clinicians, because outcomes depend on how shockwaves interact with tissue, not just that they are applied.

Shockwave therapy used by osteopaths: why the device matters
Shockwave therapy (extracorporeal shockwave therapy, ESWT) works by delivering short, high-energy acoustic pulses into tissue. These pulses trigger a cascade of mechanical and biological responses that support pain reduction and tissue repair (Schmitz et al., 2015).
However, ESWT is dose-dependent and waveform-dependent. Two key factors determine whether those biological responses occur:
Cavitation and pressure dynamics
Whether the device maintains therapeutic energy at clinically useful frequencies
This is where EMS DolorClast® systems differ meaningfully from many competitor devices.

Cavitation and tissue healing: why it matters and why device design is critical
One of the most important – and often misunderstood – mechanisms in shockwave therapy is cavitation.
Cavitation refers to the formation and controlled collapse of microscopic bubbles in fluid-rich tissue as a result of negative pressure phases in the shockwave. This process amplifies local mechanical forces and plays a key role in:
stimulating mechanotransduction in tendon and fascia
modulating pain-related nerve endings
promoting biological signalling involved in healing
High-quality experimental research has confirmed that radial shockwave devices do generate cavitation, and that cavitation is not simply “vibration” or massage (Császár et al., 2015).
Why EMS DolorClast® matters here
EMS DolorClast® devices are engineered to produce robust negative pressure phases, which are essential for meaningful cavitation. Importantly, the cavitation field produced is consistent with therapeutic tissue stimulation, rather than being incidental or negligible.
This is one of the reasons EMS systems are able to reliably trigger downstream physiological responses such as pain modulation, angiogenesis and tendon remodelling.
Frequency matters: Why some shockwave machines lose power at higher frequencies
Many clinics increase treatment frequency (Hz) to make sessions faster or more comfortable. However, research comparing ballistic (radial) shockwave devices has shown a critical issue:
Some competitor devices experience a significant drop-off in delivered pressure and energy at higher frequencies, even though the display settings remain unchanged (Reinhardt et al., 2022).
In practical terms, this means:
“10 Hz” on one machine may deliver a very different biological dose than “10 Hz” on another
At higher frequencies, some devices deliver less effective shockwave energy, potentially falling below the threshold required to stimulate tissue repair pathways

Why EMS DolorClast® stands out
Independent acoustic studies demonstrate that EMS DolorClast® systems maintain more stable output across clinically used frequencies, helping ensure that the intended therapeutic dose is actually delivered to tissue.
For patients, this means greater consistency.
For clinicians, it means better confidence that the treatment parameters used are biologically meaningful.
Focused shockwave therapy and the 5 MPa focus zone explained
In focused shockwave therapy, effectiveness is not just about “depth” – it’s about how much tissue receives a meaningful pressure stimulus.
A useful and clinically relevant concept is the 5 MPa focus zone:
This represents the three-dimensional region of tissue that experiences at least 5 megapascals of positive pressure
It provides an absolute, biologically meaningful measure of treatment volume, not just a marketing description of “focus”
Why 3D pressure distribution matters for tendon and joint healing
Shockwaves consist of:
a positive pressure phase (compression)
a negative pressure phase (rarefaction), which drives cavitation
Crucially, research has shown that in some focused shockwave devices, the spatial distribution of positive and negative pressure in three-dimensional space is not identical. This has been demonstrated in acoustic field mapping of devices such as the Storz Duolith (Perez et al., 2013).
Why this is key
If positive and negative pressure zones do not overlap well:
compression and cavitation effects may occur in different tissue regions
the biological stimulus becomes less uniform
therapeutic responses may be less predictable
In contrast, EMS focused systems are designed so that positive and negative pressure fields are more spatially congruent, meaning:
cavitation occurs where meaningful pressure is also delivered
the biological “signal” to tissue is clearer and more consistent
This matters when targeting deeper structures such as:
calcific rotator cuff deposits
deep gluteal tendons (greater trochanteric pain syndrome)
peri-articular tissues in knee osteoarthritis

Why EMS DolorClast® devices reliably stimulate key physiological pathways
Because of their pressure stability, reproducible cavitation behaviour, and well-defined focal characteristics, EMS DolorClast® systems are able to deliver a shockwave stimulus that consistently reaches the biological thresholds required to provoke meaningful tissue responses. This is a critical point for both clinicians and patients: shockwave therapy is not simply about applying a sensation to tissue, but about delivering a mechanically and biologically effective dose.
Well-designed shockwave devices must maintain their output across clinically useful frequencies, generate appropriate negative pressure phases to support cavitation, and when using focused shockwave deliver energy into a clearly defined three-dimensional treatment zone. These characteristics allow EMS DolorClast® systems to reliably engage the key, evidence-backed physiological mechanisms outlined below.
Tendon remodelling and scleraxis activation
One of the most important mechanisms underpinning shockwave therapy in tendinopathy is mechanotransduction the process by which mechanical forces are converted into cellular signals that drive tissue adaptation. When a shockwave with sufficient pressure rise time and energy reaches tendon tissue, it creates a controlled mechanical stimulus that tendon cells (tenocytes) can sense and respond to.
Experimental work has shown that shockwave therapy can influence tendon cell behaviour and gene expression, including pathways involving scleraxis, a transcription factor that plays a central role in tendon development, collagen organisation and tendon-specific extracellular matrix regulation (Zhang et al., 2011). Scleraxis is considered a key marker of tendon phenotype and remodelling capacity, and its activation supports more organised collagen alignment rather than the disorganised matrix seen in chronic tendinopathy.
The relevance of device choice becomes clear here. If a shockwave device cannot maintain sufficient pressure output particularly at higher frequencies used in clinical practice the mechanical stimulus may fall below the threshold required to activate these mechanotransductive pathways. EMS DolorClast® systems are engineered to deliver consistent acoustic output, helping ensure that tendon cells receive a stimulus capable of driving meaningful biological change rather than a purely sensory effect.

Lubricin expression and joint protection (lubricin / PRG4)
Lubricin (also known as proteoglycan 4 or PRG4) is a critical boundary lubricant produced by connective tissues and joint surfaces. It plays a vital role in reducing friction, protecting tissues from shear stress and supporting smooth movement at both tendons and joints. Reduced lubricin expression has been strongly linked to increased mechanical wear and the progression of degenerative joint conditions, including osteoarthritis.
Preclinical research has demonstrated that extracorporeal shockwave therapy can increase lubricin expression in load-bearing connective tissues, including tendons and septa, and that this response is dose-dependent (Zhang et al., 2011). This finding is particularly relevant for conditions where friction, stiffness and mechanical irritation are prominent features, such as knee osteoarthritis or chronic periarticular pain.
The ability to stimulate lubricin expression depends on delivering a shockwave that creates sufficient mechanical stress at the tissue interface without causing damage. EMS DolorClast® devices, through their controlled pressure profiles and predictable cavitation behaviour, are able to provide this stimulus in a way that aligns with the doses shown to be biologically active in experimental models. This helps explain why shockwave therapy, when appropriately applied, can improve movement tolerance and joint comfort rather than simply masking symptoms.

Substance P reduction, pain modulation and neurogenic inflammation reduction
Pain relief following shockwave therapy is not solely a placebo effect, nor does it rely exclusively on long-term structural change. One well-supported mechanism is the modulation of neurogenic inflammation, particularly through effects on Substance P, a neuropeptide involved in pain transmission and inflammatory signalling in peripheral tissues.
Substance P is commonly elevated in chronic musculoskeletal pain states and contributes to heightened nociception and persistent pain sensitivity. Experimental and clinical research indicates that shockwave therapy can reduce Substance P levels and alter the activity of pain-related nerve fibres, leading to a reduction in neurogenic inflammation and pain perception (Schmitz et al., 2009).
This mechanism helps explain why many patients experience pain relief relatively early in a course of shockwave therapy, often before full tissue remodelling has occurred. Importantly, these neuromodulatory effects appear to be linked to the negative pressure phase of the shockwave and associated cavitation phenomena. EMS DolorClast systems are specifically designed to generate these pressure characteristics consistently, supporting reliable engagement of pain-modulating pathways rather than delivering an inconsistent or sub-therapeutic stimulus.

Angiogenesis and improved blood supply
Another key physiological response to shockwave therapy is the stimulation of angiogenesis, or new blood vessel formation. Many chronic musculoskeletal conditions particularly tendinopathies and enthesopathies are characterised by poor local blood supply, which limits nutrient delivery and slows healing.
Shockwave therapy has been shown to stimulate the release of growth factors such as vascular endothelial growth factor (VEGF) and endothelial nitric oxide synthase (eNOS), promoting angiogenesis and improving microcirculation in treated tissues (Wang et al., 2003). This increase in blood supply supports tissue metabolism, waste removal and the overall healing environment.
For angiogenesis to occur, the shockwave stimulus must reach a sufficient intensity and spatial extent within the tissue. Devices that lose effective output at higher frequencies or deliver poorly defined pressure fields may fail to adequately stimulate these vascular responses. The acoustic stability and energy delivery characteristics of EMS DolorClast systems help ensure that the mechanical signal required to trigger angiogenic pathways is reliably delivered, particularly in deeper or chronically under-perfused tissues.

Calcific breakdown and resorption in chronic shoulder pain
In calcific tendinopathy of the shoulder, shockwave therapy has one of its strongest evidence bases. Multiple high-quality clinical trials have demonstrated that focused shockwave therapy can lead to resorption of calcium deposits, improved shoulder function and reduced pain, with evidence supporting a clear dose–response relationship (Ioppolo et al., 2012).
While the exact micro-mechanism is still being refined, proposed explanations include a combination of mechanical effects on the calcific deposit, biologically mediated resorption processes, and improved local tissue metabolism. What is well established clinically is that higher-quality focused shockwave delivery is associated with better outcomes than low-energy or poorly targeted treatments.
Here, the characteristics of the focused shockwave device are particularly important. Effective treatment requires a well-defined three-dimensional focus, often described using absolute pressure thresholds such as the 5 MPa focus zone, to ensure that a sufficient volume of tissue surrounding the calcification receives a therapeutic stimulus. EMS focused shockwave systems are designed to deliver energy into a predictable focal zone with more consistent overlap between positive and negative pressure fields, supporting both mechanical and biological mechanisms involved in calcific resorption.
Together, these mechanisms help explain why EMS DolorClast® shockwave systems are able to reliably stimulate the key physiological pathways associated with pain reduction, tissue repair and functional improvement. For both clinicians and patients, this reinforces a critical message: effective shockwave therapy depends on the quality and consistency of the acoustic signal delivered, not simply on the label “shockwave” itself.

Shockwave therapy for plantar fasciitis and Achilles tendinopathy in Auckland
Plantar fasciitis and Achilles tendinopathy are two of the most common reasons people in Auckland seek musculoskeletal care particularly when simple self-management strategies aren’t enough and pain limits daily activities, work or exercise. As an experienced North Shore osteopath clinic, we frequently see both conditions and integrate evidence-based treatments like shockwave therapy as part of a comprehensive care plan.
What are plantar fasciitis and Achilles tendinopathy?
Both conditions are forms of chronic load-related tissue pathology:
Plantar fasciitis (often called plantar fasciopathy) involves persistent irritation of the plantar fascia the thick connective tissue that supports the arch of the foot. Pain typically centres around the heel and is often worst first thing in the morning or after periods of rest.
Achilles tendinopathy affects the Achilles tendon at the back of the heel, leading to pain and stiffness with activity and impaired tendon resilience.
Despite differences in location, shared pathological features include:
altered tissue structure and collagen disorganisation,
reduced tendon/gliding tissue lubrication,
persistent pain signalling and neurogenic inflammation,
local vascular changes with diminished blood supply.

What this means for patients and referrers
If you’re seeking plantar fasciitis treatment in Auckland, Achilles tendinopathy treatment Auckland, or care from a North Shore osteopath, it’s reasonable to ask:
What shockwave device is being used?
Does it maintain therapeutic energy at higher frequencies?
Is the focused shockwave field well defined in three dimensions?
Is the approach based on evidence, not just machine settings?
At Movement Mechanics, our osteopaths use EMS DolorClast® shockwave systems because the physics supports the biology, and the biology supports better clinical outcomes.
Shockwave therapy is not interchangeable.
The device matters. The dose matters. And the details matter.
Jonathan Hall M.Ost, BAppSci (Human Biology), PGCertHSc (Acupuncture), GradDipHeal
Jonathan Hall is the founder and principal Osteopath at Movement Mechanics Osteopathy. Jonathan specialises in Shockwave Therapy and Western medical acupuncture. A fully qualified Osteopath registered with OCNZ, PNZ, PAANZ and ACC, Jonathan also founded Auckland Shockwave Therapy to help bring evidence-based Shockwave treatment to New Zealand using the industry-leading EMS Radial Shock Wave device.
Book an appointment with Jonathan here.
Contact Us: hello@movementmechanics.nz
References
Császár, N. B. M., Angstman, N. B., Milz, S., Sprecher, C. M., Kobel, P., Farhat, M., Schmitz, C. (2015). Radial shock wave devices generate cavitation. PLOS ONE, 10(10), e0140541.
Ioppolo, F., Rompe, J. D., Furia, J. P., & Cacchio, A. (2012). Extracorporeal shock wave therapy for supraspinatus calcifying tendinitis: A randomised clinical trial comparing two different energy levels. Physical Therapy, 92(11), 1376–1385.
Perez, C., Chen, H., Matula, T. J., Karzova, M., & Khokhlova, V. A. (2013). Acoustic field characterisation of a clinical shock wave therapy device. The Journal of the Acoustical Society of America, 134(2), 1663–1674.
Reinhardt, N., et al. (2022). Influence of pulse repetition rate on the acoustic output of ballistic pressure wave devices. Scientific Reports, 12, 1–12.
Schmitz, C., Császár, N. B. M., Milz, S., Schieker, M., Maffulli, N., Rompe, J. D., & Furia, J. P. (2015). Efficacy and safety of extracorporeal shock wave therapy for orthopaedic conditions: A systematic review on studies listed in the PEDro database. British Medical Bulletin, 116(1), 115–138.
Schmitz, C., et al. (2009). Pain relief by extracorporeal shockwave therapy: An update on the current understanding. Pain Medicine, 10(3), 505–514.
Wang, C. J., et al. (2003). Shock wave therapy induces neovascularisation at the tendon–bone junction. Journal of Orthopaedic Research, 21(6), 984–989.
Zhang, D., Kearney, C. J., Cheriyan, T., Schmid, T. M., & Spector, M. (2011). Extracorporeal shockwave-induced expression of lubricin in tendons and septa. Cell and Tissue Research, 346(2), 255–262.
Disclaimer: This content is for educational purposes and is not a substitute for professional medical advice.
© Movement Mechanics Osteopathy Auckland 2024. All rights reserved.



Comments